What is Mastitis?
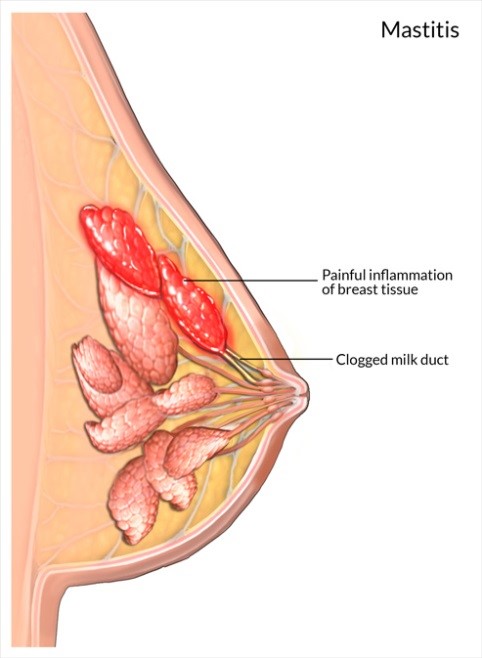
Mastitis is the inflammation of breast tissue that may present as a firm, tense area anywhere in the breast and might also appear redder and warmer than the rest of the tissue. It can also be accompanied by some whole body symptoms such as increase in temperature, aches and pains and/or fatigue.
The inflammatory response can happen with or without the presence of infection in the lactating breast. Excessive internal or external pressure on the milk duct can trigger an inflammatory response as the system tries to “fix” the affected area. There are number of management options that can support and assist the body’s natural response in dealing with the inflammation. Therefore treatment with antibiotics is not always required.
What are the symptoms?
Inflammation can cause pain, redness, swelling and heat locally on your breast.
You may also feel unwell, achy and have increased fatigue levels – similar to flu symptoms.
How can mastitis be prevented?
Ducts are small, superficial and easily compressed.
Avoid restrictive clothing or bras which may put too much pressure on breast tissue. If your clothing is leaving red marks on the skin, this may indicate it is too tight and potentially compressing milk ducts.
Always handle your breast gently and avoid squeezing your breast when baby is attaching and feeding. Remember it should never be uncomfortable or painful when handling the breast.
Make sure you keep good positioning of baby to help get good attachment and good sucking action for good milk transfer. Making yourself comfortable during the feeding can also make a big difference to baby’s attachment.
Encourage frequent, baby led feeding and avoid missing feeds and leaving long gaps between feeds
Rest, good nutrition and sleep; take any moment you can to get some relaxation and rest.
Be very aware of the way your breasts feel. Are there any general aches and pains? Feelings of hot or cold? Fever? If you ever experience feeling red, hot, swollen, engorged, painful breasts please contact your GP.
What can you do?
Continue to breastfeed normally if you can. There is no evidence of risk to the health of your baby when continuing breastfeeding with mastitis.
If you suspect you have mastitis it is recommended you are assessed by your Doctor, or Women’s Health Physiotherapist as soon as possible.
Learning to manage your symptoms is important to quickly ease your discomfort and continue breastfeeding.
Physiotherapy Management
The sooner you seek help for you symptoms the faster they will resolve.
At Innerstrength Healthcare, Therapeutic Ultrasound Therapy in conjunction with conservative management strategies, can help to improve the resolution of mastitis.
Therapeutic ultrasound (ThUS):
ThUS will assist the body in healing the breast tissue. It uses sound waves that increase cell’s permeability which will make it easier for the system to clear out the inflammation from the affected area.
Massage:
We can teach you gentle self massage techniques to assist in reduction of your symptoms.
We generally encourage you to massage upwards towards your collarbone and armpit to assist lymphatic drainage
Positioning:
Appropriate position of yourself and your baby while feeding can assist to drain the blockage
Self Management Strategies
Pain Relief
Pain relief – Panadol and Nurofen are compatible with breast feeding, if you have any medication concerns call “Medicine and Drug Information Centre” information service at the Women’s and Children’s Hospital or consult with your GP.
Feeds
Regular baby led feeding and avoid missing feeds and leaving long gaps between feeds
Directing your baby’s chin towards the blockage may help.
Remember to try out other positions such as lying on your side to feed or the football hold.
Relax and take your time when feeding.
You may choose to use your breast pump in some situations to help relieve discomfort.
Posture.
Good posture promotes good breastfeeding.
When breastfeeding in a chair: sit tall and well back in the chair.
Ensure your feet are supported (on floor, stool, phonebooks) and that your lower back is supported (eg. with a rolled up towel.)
Incorporate some neck movements and stretches to break up the constant leaning forward.
Use multiple pillows, and bring your baby to you, don’t hunch down to your baby.
Heat and cold compress
Your physio may suggest heat before feeding to assist milk flow and cold compress after to reduce inflammation.
Try applying gentle warmth to your breasts before a feed (eg. use a heat pack wrapped in a towel to provide comfortable warmth).
Do not leave on for more than 15 mins.
Try using a cold pack after a feed (eg. use a cold compress wrapped in a wet tea towel.)
Do not leave on for more than 20 mins.
Clothing
Avoid restrictive clothing or bras which may put too much pressure on breast tissue.
Handle your breast gently and avoid squeezing your breast when baby is attaching and feeding.
If your clothing is leaving red marks on the skin, this may indicate it is too tight and potentially compressing milk ducts.
Hygiene
Ensure you and others around your baby wash your hands regularly. Ensure anyone who is unwell does not come into contact with you or your baby.
Nipple damage
Monitor the health of your nipples.
To assist in healing of damaged nipple put a little breast milk onto the affected area. You may also want to temporarily use nipple shields while it heals.
Rest and Self care
Rest, good nutrition and fluids – looking after yourself is important so get as much rest as you possibly can.
Get real help! Make sure your friends and family know what your needs are now. Minimise draining visitors.
Prioritise your energy and efforts around your family (your baby, yourself and your partner).
Stress & anxiety can significantly impact on the body’s ability to repair and heal. Try our diaphragmatic breathing tracks to help with relaxation.
Exercise helps you feel good, have more energy, manage aches and pains and sleep well! Even whilst you feel unwell a 5 minute walk can help you feel better.
Breast Massage
Your physio may suggest massage
White Spot
Sometimes a white spot can develop that can be associated with Mastitis.
Your lactation consultant, GP or maternal and child health nurse can help you further with this.
The Australian Brastfeeding Assoication have a page and pictures about White Spot. Click here to read.
Lactation Consultant
Click here to find a Private Lactation Consultant in your area
Podcast
click here to listen to an excellent podcast about mastitis
Please complete the following questionnaire if you are booked in to see us for Mastitis
Inflammatory symptoms severity index


