What is Irritable Bowel Syndrome?
(Source)
If you are reading this then you absolutely know lots about Irritable bowel syndrome already.
You are probably more interested in what to do about it.
Irritable Bowel Syndrome has been charactersied as type of "functional bowel disorder."
It is a chronic gastrointestinal (gut) disorder characterised by fluctuating abdominal pain or discomfort.
It is associated with an altered bowel habit.
It occurs in the absence of structural changes in organs or tissues.
More detail below.
What are Functional Bowel Disorders?
A functional disorder is defined as medical condition that impairs the normal function of a bodily process.
A functional disorder is different from other health problems as every part of the body looks completely normal under examination, dissection or even under a microscope.
Functional bowel disorders is an official name for gut problems that include:
ongoing abdominal pain,
bloating,
distention,
and/or bowel habit abnormalities (constipation, diarrhea, or mixed constipation and diarrhea).
They are distinguished from other gut problems in that they:
occur for at least 6 months
are present during the last 3 months
occur at least 1 day per week
and no obvious abnormalities found with routine diagnostic examinations.
They are classified into 5 categories:
Irritable bowel syndrome (IBS),
Functional constipation (FC),
Functional diarrhea (FDr),
Functional abdominal bloating/distention, and
Unspecified FBD (Source)
How is Irritable Bowel Syndrome diagnosed?
It is usually diagnosed by a gastroenterologist.
They rule out the following conditions using clinical history, physical examination, minimal laboratory tests, and sometimes a colonoscopy.
- Inflammatory bowel disease (IBD)
- Celiac disease (make sure when you have the test that you have been eating gluten)
- Lactose and fructose intolerance
- Microscopic colitis
Diagnostic Criteria for Irritable Bowel Syndrome
Recurrent abdominal pain, on average, at least 1 day per week in the last 3 months, associated with 2 or more of the following criteria:
1. Related to defecation
2. Associated with a change in frequency of stool
3. Associated with a change in form (appearance) of stool
Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis.
Different types of Irritable Bowel Syndrome
There are four subcategories of IBS:
- Predominant constipation(IBS-C),
- Predominant diarrhea (IBS-D),
- Mixed bowel habits (IBS-M),
- IBS unclassified (IBS-U)
How Common is Irritable Bowel Syndrome?
It is estimated that the world wide 11.2% suffer with Irritable Bowel Syndrome.(Source)
Managing Irritable Bowel Syndrome
The first thing to know is that if you are diagnosed with IBS it is a very bothersome but not dangerous problem.
We know that most people with Irritable bowel syndrome are inundated with advice.
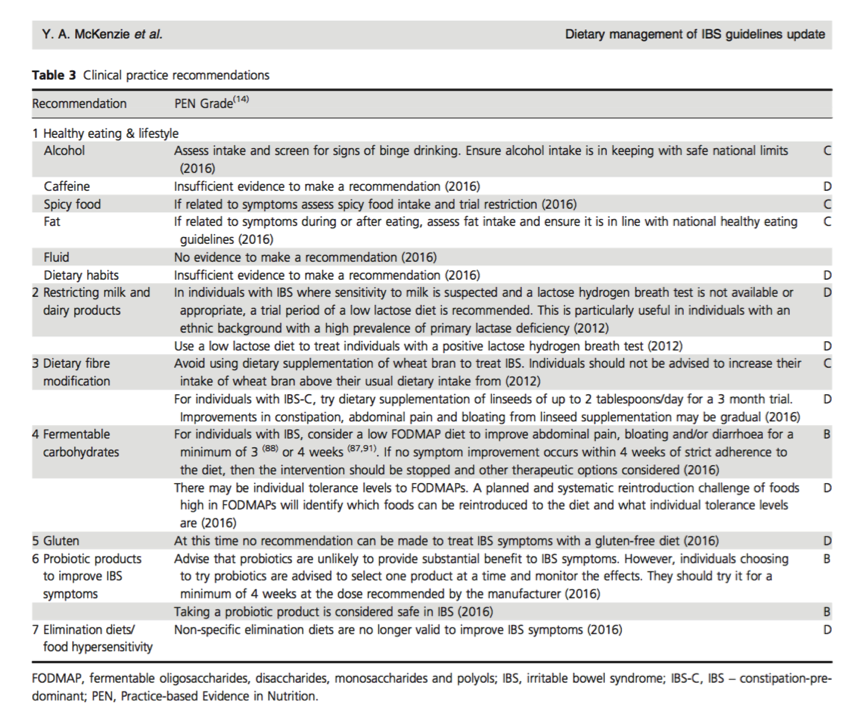
Below is a summary of the latest evidence from two very well researched sources. (Source) (Source)
| Grading | Description |
| Level A | the conclusion is supported by good evidence |
| Level B | the conclusion is supported by fair evidence |
| Level C | the conclusion is supported by limited evidence or expert opinion |
| Level D | evidence is limited |
Start with Healthy Eating and Lifestyle including exercise, stress reduction, and attention to impaired sleep.
- Alcohol - Alcohol is thought to affect gut muscle, absorption and gut barrier function. Alcohol can induce or worsen IBS symptoms (C.)
- Caffeine - Caffeine increases gastric acid juices and large intestine muscle activity in healthy subjects. Caffeine can induce or worsen IBS symptoms (D.)
- Spicy food - Capsaicin is the active component in hot peppers and, in spicy food, this compound is responsible for accelerating gut travel transit via the receptor "TRPV" causing abdominal pain and burning sensations in healthy individuals. Increased TRPV receptors have been found in individuals with gut hypersensitivity (C.)
- Fat - Fat stimulates the gastrocolic reflex (between gut and intestine motion) and, when delivered directly into the duodenum, the response is prolonged and exaggerated in individuals with IBS. Fat increased IBS symptoms (C.)
- Fluid intake - Increase fluid minimum 1.5 -2L per day to improve Functional Constipation (No research) Small studies have shown that there is no benefit in increasing fluid intake in those who are hydrated normally.
- Healthy Balanced Diet (D.)
- Restrict milk and diary (C.) Needs careful assessment by allergy experienced dietician or doctor to reduce risk of dietary imbalance.
- Mintec - there is some evidence Mintec is effective for predominantly abdominal pain - works as an anti spasmodic. Take 1h before meals not after. Can take 1-2 capsules up to 3 times per day
If symptoms persist then see Dietician Sally Morgan at Innerstrength Physiotherapy.
What are FODMAPS?
One of the underlying causes of IBS can be FODMAPS.
Before you alter your diet it is advisable to talk to Dietician Sally Morgan at Innerstrength Physiotherapy.

Managing functional constipation with diet and lifestyle
Increase dietary fibre and fluid
A daily fiber intake of 25 g/day can increase stool frequency and decrease laxative use in people with functional consitpation and you can enhance this enhanced by increasing fluid intake to 1.5-2.0 liters/day. (Source)
For help with dietary changes see our Dietician Sally Morgan at Innerstrength Physiotherapy
Fibre supplements
Fibre supplements are a first-line therapy for chronic idiopathic constipation. (Source)
They are food products and therefore are relatively safe, inexpensive and are widely available.
However up to 50% of users will be dissatisfied with their effect due to flatulence and bloating.
They reduce colorectal cancer risk compared to nonfibre laxative use.
Which Fibre Supplement is Likely to be more effective?
It remains unclear which type of fibre is the most useful, although the most evidence seems to be for psyllium (a soluble, nonprebiotic fibre).
How much fibre supplement should I take?
Doses >15 g are more effective for chronic constipation.
What are Psylium Husks?
The most robust evidence for an individual fibre seems to be for psyllium (a nonprebiotic).
Psyllium (ispaghula husk), obtained from the seeds of plantago ovata, is a soluble viscous fibre with a high water-holding capacity that normalises stool form.
Stool water content has been highly associated with stool consistency, and a relatively small increase in stool water content has been shown to result in a relatively large stool softening effect.
In contrast, psyllium is only partially fermented in the gut and the stool softening effect is a direct consequence of its ability to form a gel and hold many times its own weight in water.
Psyllium showed greater effect on stool consistency compared to prebiotics (GOS and inulin). What are Prebiotics?
This compared favourably with both osmotic laxatives, including polyethylene glycol (~17 g once or twice daily), and stimulant laxatives [e.g. bisacodyl (10 mg)] significantly increased stool frequency.
Metamucil contains psyllium husk and one teaspoon contains 2.4g of fibre.
Psyllium husks are available in supermarkets.
Physical activity
There is evidence that prolonged inactivity is a cause of constipation so get moving and follow the current guidelines for exercise.(Source)
Make sure you do 30 minutes of moderate intensity exercise on most days.
Manintaining a regular morning routine.
Bowel contractions are maximal on waking up and after a meal or warm drink (the gastro-colic response.)
Try and optimize this with scheduled gentle attempt at defecation after a warm drink and breakfast.
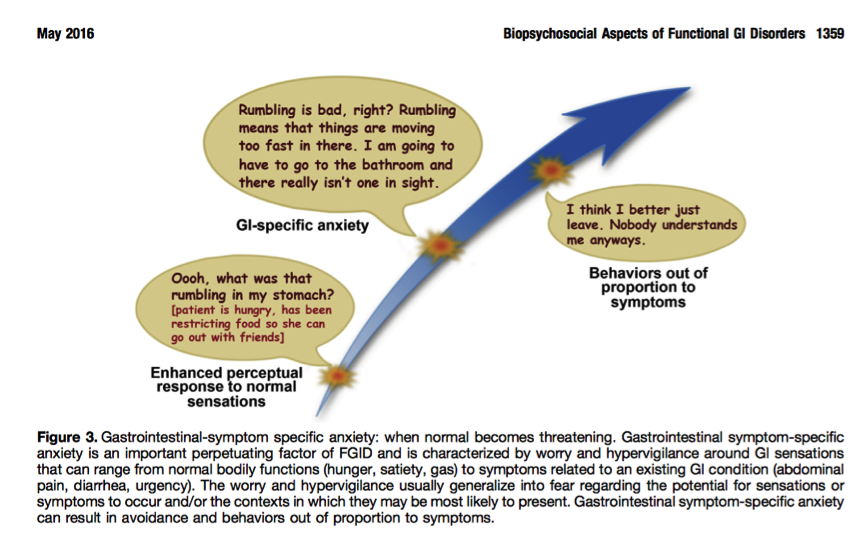
Role of Stress, Anxiety and Hypervigilance in Gut Problems
Evidence and understanding of the role of stress in gut problems is growing.
Most people with gut problems understand that when psychological stress increases so too do gut complaints.
One study found that the level of chronic life stress threat predicts the outcome in most people with Irritable Bowel Syndrome and dyspepisa. (Source)
Those who improved did so in the absence of chronic stressors.
One study showed inflammation of the gut wall with Diarrhorea predominant Irritable Bowel Syndrome.(Source)
Below is also a picture of how thoughts and anxiety can contribute to suffering with bowel suffering.
How do I manage stress with my gut problems?
Hypnosis and Psychology are now recognised treatments in the management of functional Bowel Disorders
The type of therapies are hypnosis, mindfullness meditation, aceptance committment theories and cognitive behavioural therapies.
Jo Sheedy Psychologist at Innerstrength Phsyiotherapy is happy to help.
Diaphragmatic Breathing has an audio track that you can use to interupt some of the thoughts and interupt your focus on your gut.
Another article https://www.nps.org.au/australian-prescriber/articles/treatment-of-irrit...

